Tip your HAT to Sepsis
50% of the sepsis related deaths in children occur in the first 24 hours. 60% of Australians have never heard of sepsis with only 14% being able to name the symptoms with newborns and young children most vulnerable to sepsis. (CEC QLD 2020). Not only does sepsis come with a high mortality rate, but many patients who do survive are left with life changing effects such as amputations, sensory losses, chronic pain, fatigue and post-traumatic stress syndrome.
Early recognition and management of sepsis saves lives. So how do we recognise sepsis?
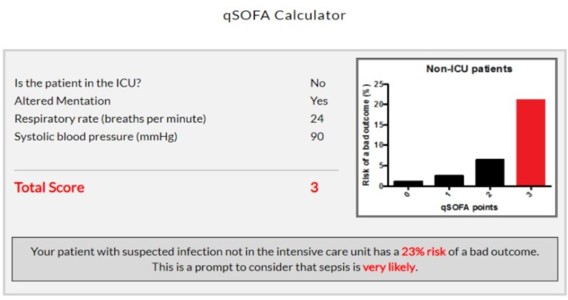
The qSOFA score is a bedside tool that clinicians can use to identify possible sepsis in patients with suspected infections. Patients who demonstrate two or more of these symptoms are at greater risk of deterioration with a poor outcome outside the ICU. The qSOFA uses three criteria of:
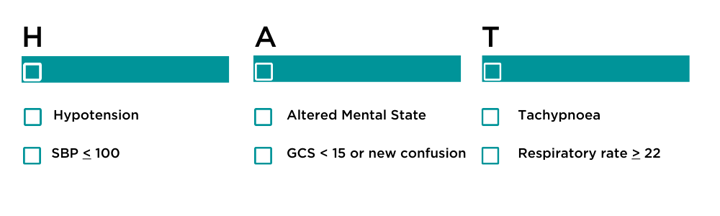
If these criteria are applied to patients with known or suspected infections, then the question should be asked "Could this be Sepsis?"
Do you want to know the risk of a bad outcome for your patient with sepsis? Use the qSOFA calculator at www.qsofa.org
So why is sepsis such a problem?
In response to infection the body’s immune system responds. An inflammatory response to infection starts the clotting cascade with an increase in coagulation and decrease in fibrinolysis. This impedes circulation with reduced blood flow and oxygen to cells causing organ dysfunction.
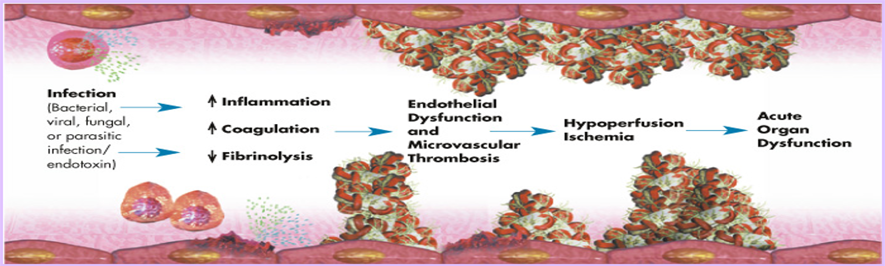
Source: ( Eli Lilly and Company: Surviving Sepsis Education Program. Adapted from Bernard et al 2001)
The Inflammatory response to infection
As the patient experiences tissue hypoxia, lactate levels will rise in response to anaerobic metabolism. This is why lactate is often considered a marker of sepsis. However it is important to remember that elevated lactate is seen in many clinical conditions, and should not be used as ONLY a measure of sepsis.
Lactate can be a useful measure to assess for a metabolic response to septic shock and guide treatment. Patients with septic shock can be identified as those patients with persistent hypotension despite adequate fluid resuscitation. Septic patients with a MAP ≤ 65mmHg and a serum lactate > 2mmol/L now have a mortality rate >40%. These patients will need vasopressor support.
How do we treat?
Source control is the cornerstone of sepsis management, the only way to ‘cure’ sepsis is to identify and remove the source. With consideration to antimicrobial stewardship, the early administration of antibiotics is thought to reduce mortality. The gold standard is to administer antibiotics within an hour of signs of sepsis, with every hour antibiotics are delayed, mortality increases by 8%. Antibiotics should be reviewed every 24hrs.
Related courses
This article last reviewed by Susan Helmrich August 2023.
References and Additional Reading:
https://www.australiansepsisnetwork.net.au/ssnap
https://www.cec.health.nsw.gov.au/keep-patients-safe/deteriorating-patient-program/sepsis
https://clinicalexcellence.qld.gov.au/resources/sepsis
https://sepsistrust.org/professional-resources/
https://www.sccm.org/SurvivingSepsisCampaign/Guidelines
Dellinger, R.P., Levy, M.M., Rhodes, A. et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock, 2012. Intensive Care Med 39,165–228 (2013). https://doi.org/10.1007/s00134-012-2769-8
Raith EP, Udy AA, Bailey M, et al. 2017 Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA; 317: 290-300 https://doi.org/10.1001/jama.2016.20328
Rob G. H. Driessen, Nanon F. L. Heijnen, Riquette P. M. G. Hulsewe, Johanna W. M. Holtkamp, Bjorn Winkens, Marcel C. G. van de Poll, Iwan C. C. van der Horst, Dennis C. J. J. Bergmans & Ronny M. Schnabel (2021) Early ICU-mortality in sepsis – causes, influencing factors and variability in clinical judgement: a retrospective cohort study, Infectious Diseases, 53:1, 61-68, DOI: 10.1080/23744235.2020.1821912
Rudd KE, Johnson SC, Agesa KM, et al. 2020 Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet 395: 200-211 https://doi.org/10.1016/S0140-6736(19)32989-7
Singer M, Deutschman CS, Seymour CW, et al. 2016 The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA; 315: 801-810 https://doi.org/10.1001/jama.2016.0287

Susan is the Head of Nursing Education for the Medcast Group.
DipAppScNsg, BN, CritCareCert, CoronaryCareCert, TraumaNsgCareCert, CertIV(TAE), MN(Ed), and GradCert(Ldrshp & Mgt).
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreFollow James, a 7-year-old boy scheduled for a tonsillectomy and adenoidectomy, as we explore how the 4 P’s of child preparation – Prepare, Play, Parent, Praise – can be used in day surgery to reduce procedural anxiety, support family-centred care, and improve the overall patient experience
Caregiver concern is a powerful predictor of clinical deterioration in children, often surpassing abnormal vital signs. A recent Lancet study confirms its association with ICU admission and ventilation. Integrating caregiver input into assessments, documentation, and escalation protocols can significantly improve early recognition and outcomes in paediatric emergency care.
Sepsis is a time-critical medical emergency. The National Sepsis Program urges GPs and primary care clinicians to enhance early recognition and management of sepsis to save lives. This update outlines key actions and available resources to support timely diagnosis and intervention across primary care settings.
