The first five minutes - prioritising care in the ICU
Your patient, Anna, has just arrived in the intensive care unit from the operating room where she had an anaphylactic arrest at the completion of her total hip replacement surgery. There will be a range of actions that need to be prioritised to ensure a safe transition of care, optimisation of recovery, and minimisation of risk of deterioration or re-arrest. What are your priorities?
1. Preparation
Prior to patient arrival, ensure the ICU environment is optimally prepared for rapid response:
-
Check emergency equipment: Check bedside and emergency equipment is ready for use. This should include suction, oxygen, and resuscitation trolley. Specialist equipment like ventilators should also be checked and put into standby mode prior to the patient arriving.
-
Set up monitoring parameters: Adjust alarms on monitors based on the patient’s expected condition. Plan for a likely insertion of central line, arterial line, and IDC. If you have been updated on the patient’s haemodynamic status, you may be able to start preparing any required infusions such as noradrenaline.
2. Admission and rapid primary assessment
The first few minutes with an unstable ICU patient are crucial.
-
Obtain handover via a clinical handover tool like ISBAR. Check any devices including IV access, drains, IDC, or nasogastric tube.
-
Attach monitoring and verify alarm parameters are appropriate.
-
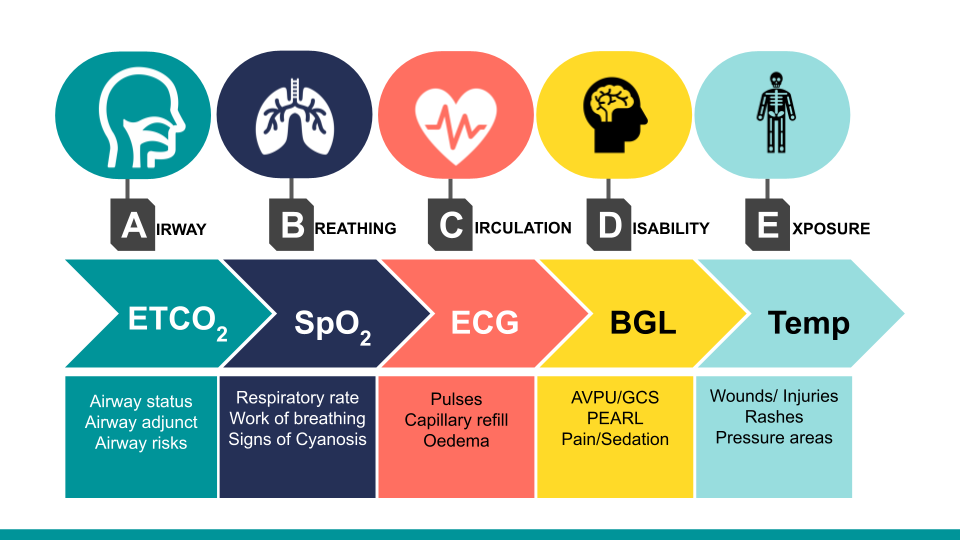
Perform a primary survey using an ABCDE (airway, breathing, circulation, disability, exposure) approach.
-
Document assessment findings and baseline observations.
3. Establish priority interventions
While stabilising the patient, work with the multidisciplinary team members to prioritise care including insertion of lines, and devices, performing x-rays and bloods, and obtaining an ABG and 12 lead ECG. Prioritise based on patient requirements and stability:
-
Fluid resuscitation and vasopressors: In cases of haemodynamic instability, prompt administration of IV fluids and titration of vasopressors, like noradrenaline, can improve tissue perfusion.
-
Central venous line insertion: For patients who require continuous vasopressors and inotropes, a central line should be prioritised to ensure effective administration and allow for haemodynamic monitoring.
-
Ventilation support: For patients with respiratory failure, start high-flow nasal prong oxygen (HFNP) or non-invasive ventilation (NIV), or mechanical ventilation. The decision between the two depends on the severity of hypoxaemia and dyspnoea.
4. Monitoring and reassessment
Continual monitoring is necessary to track the response to interventions and detect deterioration early:
-
Haemodynamic stability: Reassess blood pressure, heart rate, and perfusion frequently, adjusting vasopressor support as needed.
-
Ventilation and oxygenation: Monitor oxygen saturation and adjust oxygen delivery to maintain target SpO₂ levels, particularly if the patient is on NIV or mechanical ventilation.
-
Neurological status: Regular assessment of neurological function, including responsiveness and Glasgow Coma Scale (GCS) score, is vital to detect any signs of deterioration.
5. Promoting a safety culture
A commitment to patient safety is essential, particularly when managing unstable patients. The Australian College of Critical Care Nurses (ACCCN) recommends cultivating a culture where asking for assistance and utilising clinical support resources is encouraged. Reaching out to ICU team leaders or senior clinicians can provide additional perspectives and help guide complex decisions.
Related courses

Susan is the Head of Nursing Education for the Medcast Group.
DipAppScNsg, BN, CritCareCert, CoronaryCareCert, TraumaNsgCareCert, CertIV(TAE), MN(Ed), and GradCert(Ldrshp & Mgt).
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreFollow James, a 7-year-old boy scheduled for a tonsillectomy and adenoidectomy, as we explore how the 4 P’s of child preparation – Prepare, Play, Parent, Praise – can be used in day surgery to reduce procedural anxiety, support family-centred care, and improve the overall patient experience
Caregiver concern is a powerful predictor of clinical deterioration in children, often surpassing abnormal vital signs. A recent Lancet study confirms its association with ICU admission and ventilation. Integrating caregiver input into assessments, documentation, and escalation protocols can significantly improve early recognition and outcomes in paediatric emergency care.
Sepsis is a time-critical medical emergency. The National Sepsis Program urges GPs and primary care clinicians to enhance early recognition and management of sepsis to save lives. This update outlines key actions and available resources to support timely diagnosis and intervention across primary care settings.