James presents with acute shortness of breath and a wheeze during a summer soccer match - clinical opal
James, a 22 year old university student, presents to the emergency department with sudden-onset shortness of breath, chest tightness, and wheezing that started during a uni soccer game played in a recently mowed field just before a late afternoon summer storm hit the area. James has a history of mild seasonal allergic rhinitis but has never been diagnosed with asthma and says his symptoms became intense very quickly, leaving him anxious and struggling to breathe.
Is James experiencing thunderstorm asthma?
Yes, his history of seasonal allergic rhinitis, coupled with his presenting symptoms and potential exposure to grass pollens immediately before a thunderstorm indicate the likelihood of thunderstorm asthma.
Patients like James are at risk of thunderstorm asthma particularly when pollen counts are high during storm season
In November 2016, Melbourne experienced the worst epidemic thunderstorm asthma event recorded in the world. This major health crisis saw emergency services overwhelmed with calls regarding respiratory distress, resulting in tragic outcomes.
The symptoms of thunderstorm asthma occur suddenly and severely. This condition is caused by a combination of high pollen levels - in Australia, this is typically rye grass pollen - and specific weather patterns. The changing pressure system causes pollen grains to be drawn upwards into the clouds where they absorb water and burst. These small allergen particles can then be carried long distances on the wind and are pushed back to the ground, where they are inhaled. Due to the size of these particles, they penetrate further into the airways, resulting in particularly severe respiratory symptoms.
Key risks of thunderstorm asthma:
Thunderstorm asthma typically affects individuals with underlying seasonal allergies or undiagnosed asthma but can also occur in patients without asthma. Risk factors include:
-
exposure to high pollen levels
-
recent thunderstorms
-
a history of hay fever or seasonal allergies
-
lack of preventive asthma management in individuals with known asthma
Patients of any age can be affected.
Grass pollen season in Australia, and the period of highest risk of an epidemic thunderstorm asthma event, is considered to be between 1st October and 31st December.
Differentiators between thunderstorm asthma and acute asthma:
While acute asthma generally results from known triggers in asthmatic patients, thunderstorm asthma episodes are unique in their association with high pollen counts and specific weather conditions. Thunderstorm asthma can occur suddenly and intensely even in people without a prior asthma diagnosis and tends to affect many people simultaneously due to the widespread nature of the environmental trigger. In contrast, typical acute asthma presentations are usually less influenced by sudden environmental factors and more by personal triggers.
Key symptoms include:
-
sudden-onset shortness of breath
-
wheezing and chest tightness
-
persistent cough
Management of thunderstorm asthma
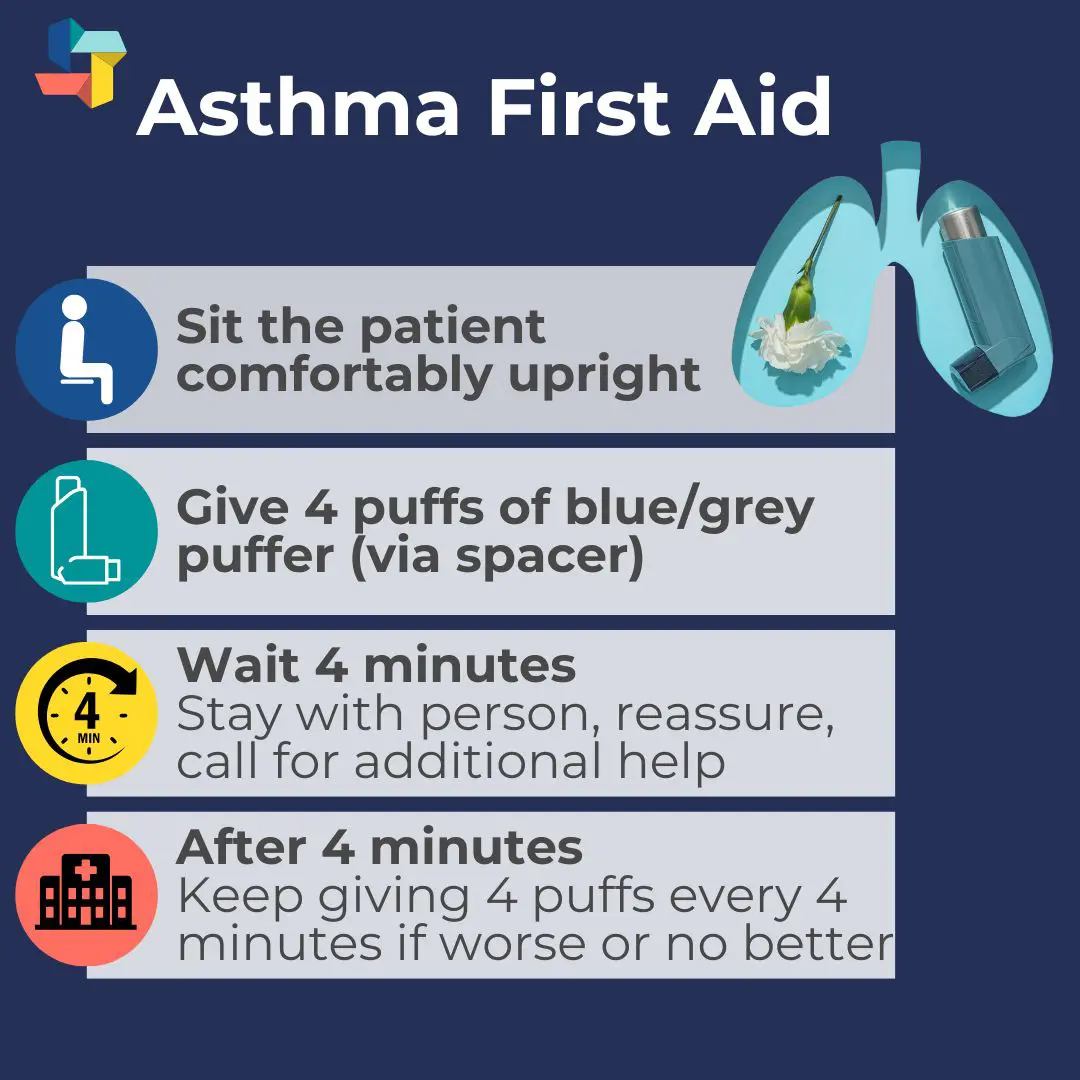
Follow standard asthma protocols using the asthma first aid steps:
Severe cases may require oxygen therapy, continuous bronchodilator administration and systemic corticosteroids. In cases where the patient is unresponsive to initial treatments, escalation to higher levels of care is recommended.
Patient education includes developing an asthma management plan, which can involve the use of preventative puffers, especially during high pollen season, and limiting outdoor activities during times of high risk. Patients may also benefit from thunderstorm asthma alerts, and monitoring pollen forecasts and thunderstorm warnings.
Related courses

Susan is the Head of Nursing Education for the Medcast Group.
DipAppScNsg, BN, CritCareCert, CoronaryCareCert, TraumaNsgCareCert, CertIV(TAE), MN(Ed), and GradCert(Ldrshp & Mgt).
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreMyMedicare is now part of routine general practice, with practical implications for billing, continuity of care, and practice systems. This FastTrack clarifies important points regarding eligibility, impacts on the GPCCMP billing, and how to avoid rejected claims. 30mins each RP and EA available.
Many GPs may not see veterans frequently. This FastTrack provides a summary of key steps that can make veteran care efficient, rewarding and well-integrated into routine practice, including links to additional resources. 30mins each of RP and EA are available.
From the 1st Nov 2025, updates to the MBS affect all GPs providing services related to long-acting reversible contraceptives. This FastTrack will get you up to date on which items attracted an increased rebate, the new item number, and how to avoid common compliance pitfalls. 30mins each of RP and EA CPD available with the quiz.
