Reproductive genetic carrier screening - clinical fact sheet and MCQ
![]()
Reproductive genetic carrier screening (RGCS) is a type of genetic testing offered to individuals and their reproductive partners (including sperm or egg donors) to determine the chance of having a child with one of the screened inherited conditions. These are typically autosomal recessive (AR) and X-linked (XL) conditions that present in infancy or childhood and result in serious health complications.
In Australia, 1 in 20 people are carriers one of the three most common genetic conditions: cystic fibrosis (CF), spinal muscular atrophy (SMA) and fragile X syndrome (FXS)[1]. This equates to a 1 in 240 chance of both reproductive partners being a carrier for one of these three conditions[1]. If both reproductive partners are a carrier for the same AR condition, or the female reproductive partner is a carrier for an XL condition, there is a 1 in 4 chance of having an affected child.
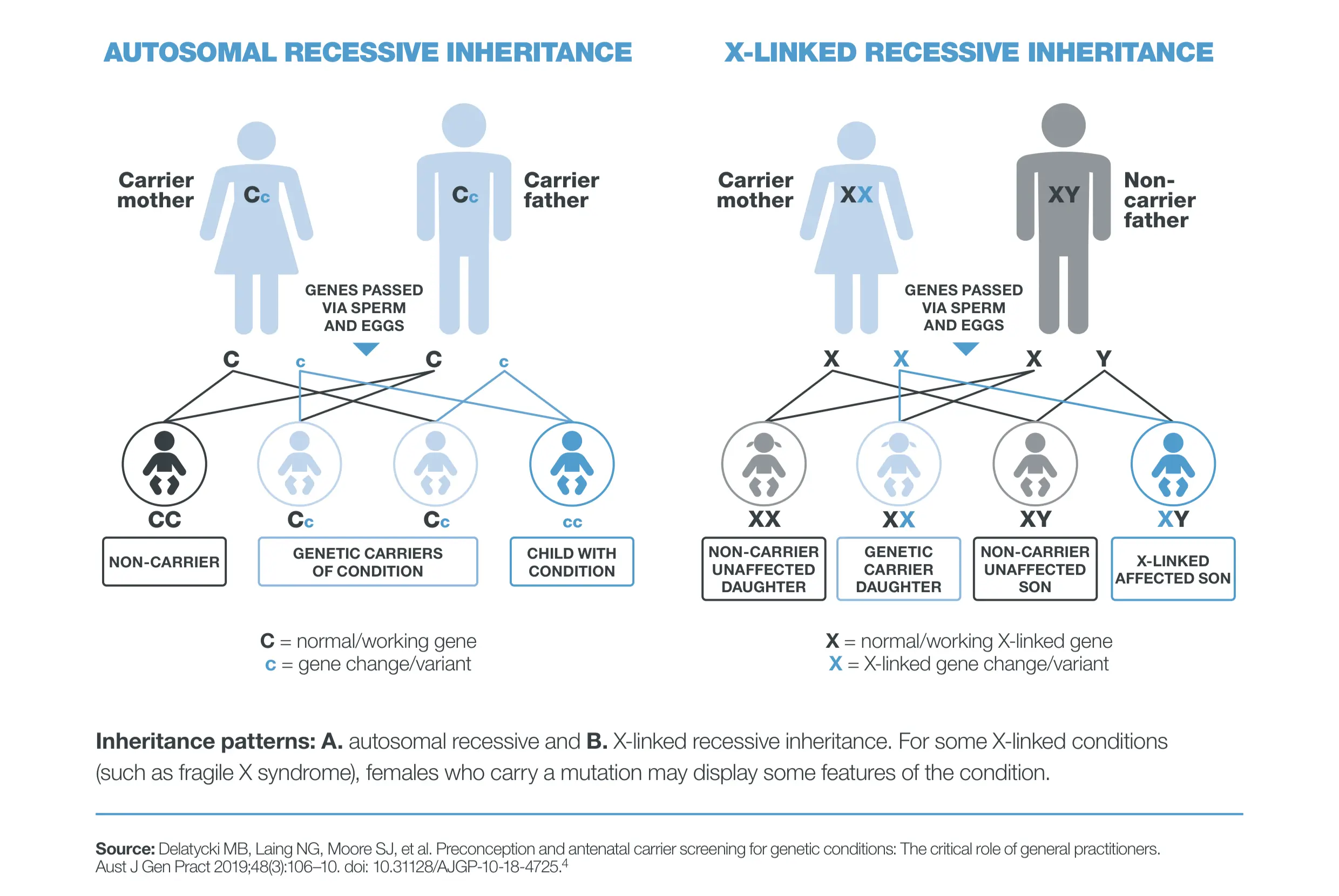
Image 1: autosomal recessive and X-linked inheritance patterns (source: https://www.racgp.org.au/getmedia/db5d54a8-1e8c-4c3f-9b8b-51fa457c767c/Genetic-carrier-screening_1.pdf.aspx)
Who should be offered RGCS
RANZCOG recommends that information on RGCS should be offered to all people planning a pregnancy, or in the first trimester of pregnancy, whether or not there is a known family history of a genetic condition[2].
When should RGCS be offered
It should be offered pre-pregnancy or in the first trimester of pregnancy.
Testing options
1. Three-gene panel
-
This panel screens for three inherited genetic conditions in Australians - CF, SMA and FXS
-
All females are able to access a Medicare Benefits Schedule (MBS) rebate for this test (MBS item 73451) so there is no out-of-pocket cost
-
Male reproductive partners can also access a MBS rebate (MBS item 73452) for CF and SMA screening if the female reproductive partner is confirmed as a carrier of one of those AR conditions
|
Condition |
Approximate carrier frequency |
Approximate incidence |
|---|---|---|
|
CF |
1 in 34 |
1 in 4,925 |
|
SMA |
1 in 50 |
1 in 9,917 |
|
FXS |
1 in 330 |
1 in 7,143 males |
2. Expanded panel
-
This panel screens for hundreds of AR and XL conditions (including CF, SMA and FXS) involving over 1,000 genes selected due to the severity of conditions and childhood onset
-
This panel offers the most comprehensive screening option for reproductive partners
-
There is no MBS rebate and people will pay an out-of-pocket fee
-
Screening can be performed sequentially (screen the female first and then screen the male reproductive partner if the female partner is a carrier of an AR condition) or concurrently (screen both reproductive partners at the same time)
-
Concurrent testing is more time-efficient, but also more expensive
-
Laboratories differ regarding the number of conditions and genes screened as well as the cost and the turnaround time of the test
- No single pathology provider or testing laboratory is recommended over any other and offerings change frequently. A list of available pathology providers can be found at this link and is current at the time of publication.
Pre-test counselling
This should cover:
-
RGCS is optional but recommended for all people planning a pregnancy or in the early stages of pregnancy whether or not there is a known family history of a genetic condition
- The expanded panel is the most comprehensive screening option
-
limitations of RGCS
-
-
not all conditions, genes, or gene changes are included – a ‘low chance’ result does not exclude all risk
-
it does not screen for chromosomal conditions, such as Down syndrome, in a pregnancy. Non-invasive prenatal testing/screening (NIPT/S) is available for this purpose.
-
Interpreting the results
The below table outlines the possible results.
|
Combination |
Female/egg carrier status |
Male/sperm carrier status |
Chance of an affected child |
Referral to genetic service |
|---|---|---|---|---|
|
AR |
Carrier for an autosomal recessive condition |
Carrier for the same autosomal recessive condition |
Increased 1 in 4 (25%) |
Yes |
|
AR |
Carrier for an autosomal recessive condition |
Not carrier for the same autosomal recessive condition |
Low |
No |
|
AR |
Not carrier for an autosomal recessive condition |
Not carrier for the same autosomal recessive condition |
Low |
No |
|
AR |
Carrier for an autosomal recessive condition |
Not tested for the same autosomal recessive condition |
Unclear Arrange testing for the same autosomal recessive conditions in the partner |
No Do not refer before partner |
|
XL |
Carrier for an X-linked condition |
Not carrier for an X-linked condition or untested |
Increased 1 in 4 (25%) |
Yes |
|
XL |
Not carrier for an X-linked condition |
Not carrier for an X-linked condition or untested |
Low |
No |
Post-test counselling
Post-test counselling topics differ based upon the combination of results received for the reproductive partners.
1. Low chance results
-
Provide reassurance, while clearly communicating residual risk
-
Emphasise the importance of first and second trimester anatomy ultrasounds and standard antenatal care
-
Public genetics services typically do not accept referrals for low chance results. If required, consider private genetic counselling or the referral pathway for genetic counselling offered by the testing provider. A list of private genetic services can be found here
2. Increased chance results
- People should be referred to a clinical genetics service for comprehensive genetic counselling. If a patient is already pregnant, this referral should be marked urgent and expedited
- Your patient’s local clinical genetics service can be identified here[3]
- Reproductive options for non-pregnant patients include in vitro fertilisation (IVF) with preimplantation genetic diagnosis/testing (PGD/T)[4], prenatal diagnostic testing via chorionic villus sampling or amniocentesis[5], use of donor gametes, adoption, or electing not to have children
- Cascade screening should also be recommended for at-risk relatives
3. If a fragile X premutation is identified:
- there are associated personal health implications for individuals with a fragile X premutation, where the FMR1 gene contains 55 to 200 CGG repeats
- female premutation carriers of FXS may develop fragile X-associated primary ovarian insufficiency (FXPOI) whilst female and male premutation carriers may develop fragile X-associated tremor/ataxia syndrome (FXTAS)[6]
- these patients should be referred to clinical genetics for further evaluation and discussion regardless of their chance of having an affected child
References
-
Dalton Archibald A, Smith MJ, Burgess T, et al. Reproductive genetic carrier screening for cystic fibrosis, fragile X syndrome, and spinal muscular atrophy in Australia: outcomes of 12,000 tests.Genet Med;2018;20(5):513-523.
-
Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). Genetic carrier screening. Melbourne: RANZCOG; 2024. Available at: https://ranzcog.edu.au/wp-content/uploads/Genetic-Carrier-Screening.pdf. (last accessed August 2025).
-
Centre for Genetics Education. Genetic services. Sydney: NSW Health; 2022. Available from: https://www.genetics.edu.au/SitePages/Genetic-Services.aspx. (last accessed August 2025).
-
Centre for Genetics Education. Pre-implantation genetic diagnosis. Sydney: NSW Health; 2022. Available from: https://www.genetics.edu.au/publications-and-resources/facts-sheets/fact-sheet-17-preimplantation-genetic-diagnosis. (last accessed August 2025).
-
Centre for Genetics Education. Diagnostic tests during pregnancy. Sydney: NSW Health; 2022. Available from: https://www.genetics.edu.au/publications-and-resources/facts-sheets/fact-sheet-18-diagnostic-tests-during-pregnancy. (last accessed August 2025).
-
Fragile X Association of Australia. Fragile X permutation carriers. 2025. Available at: https://www.fragilex.org.au/understanding-fragile-x/fragile-x-premutation-carriers/. (last accessed August 2025).
Claim your CPD
After reading the clinical summary above and reviewing the references, complete the quiz to gain 30 minutes of EA CPD and 30 minutes of RP CPD.
You can either self-report CPD to your CPD home, or Medcast will track your learning via your personal CPD Tracker and you can download and report these points once a year. See our CPD Tracker FAQ.
Quiz
Please log in or sign up for a free Medcast account to access the case study questions and achieve the CPD credits.

Many GPs may not see veterans frequently. This FastTrack provides a summary of key steps that can make veteran care efficient, rewarding and well-integrated into routine practice, including links to additional resources. 30mins each of RP and EA are available.
From the 1st Nov 2025, updates to the MBS affect all GPs providing services related to long-acting reversible contraceptives. This FastTrack will get you up to date on which items attracted an increased rebate, the new item number, and how to avoid common compliance pitfalls. 30mins each of RP and EA CPD available with the quiz.
GPs are often faced with the presentation of a red, sticky eye. Even without a slit lamp, there are key points in your clinical assessment that can help to differentiate the causes of conjunctivitis and guide the appropriate management. Read the fact sheet then claim 30mins each of RP and EA CPD with the quiz.

