Preoperative Assessment and Mallampati Scores
A preoperative assessment by anaesthetic staff should include the Mallampati Score, as there is a direct correlation between the amount of space in the pharynx and the laryngoscopic view during intubation which has been refined by Cormack and Lehane (1984).
This can assist in predicting patients who may have a difficult intubation and preparation with additional equipment. It is important to note, regardless of the Mallampati Score, that difficult intubation can occur without warning, and access to a difficult airway trolley is essential in operating theatres.
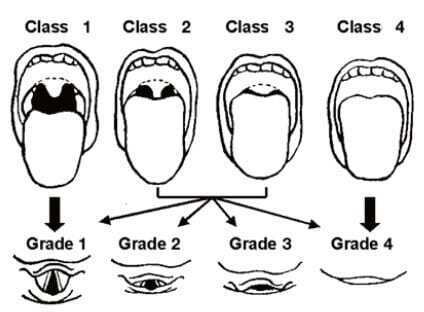
To assess the patient for their Mallampati Score, ask them to sit upright and open their mouth fully with their tongue protruding.
The structures that can be visualised classify the patient’s score. The less pharyngeal structures that can be seen results in a higher score or classification, which in turn predicts increasing difficulty in achieving intubation, however in another study conducted by Lee et al. (2000), the Mallampati score did not predict difficult bag-valve-mask ventilation. Interestingly, the Mallampati Score can also be used to assess a patient’s risk of Obstructive Sleep Apnoea (Wickramasinghe, 2020).
The scoring classification is as follows with visualisation of:
Class 1: soft palate, uvula and faucial pillars
Class 2: soft palate, majority of uvula and part of faucial pillars
Class 3: part of soft palate, base of uvula
Class 4: hard palate only
Related courses
If you are interested in learning more, our suite of Anaesthesia and Recovery Nursing courses cover a wide range of topics.
- Perioperative Professional Practice and the Patient Jouney: Perioperative Nursing Update Module 1
- Anaesthesia and Recovery Nursing: The Essentials
- Anaesthesia and Recovery Nursing in the Day Surgery Environment
- Anaesthesia and PACU Nursing (topics change every 12 months)
By Crystal Smith and Ken Hambrecht.
References:
Cormack, R.S.; Lehane, J. (1984). Difficult tracheal intubation in obstetrics. Anaesthesia. 39 (11): 1105–11. doi:10.1111/j.1365-2044.1984.tb08932.x. PMID 6507827.
Lee, A; Fan, LT; Gin, T; Karmakar, MK; Ngan Kee, WD (Jun 2006). A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesthesia and Analgesia. 102 (6): 1867–78. doi:10.1213/01.ane.0000217211.12232.55. PMID 16717341.
Mallampati, SR, Gatt, SP, Gugino, LD, Desai, SP, Waraksa, B, Freiberger, D & Liu, PL. 1985. A clinical sign to predict difficult tracheal intubation: a propensity study. Can Anaesth Soc J; 32 (4) July, doi:10.1007/FB03011357.
Shehzad, A & Cadogan, M. 2020. Mallampati Score. Life in the Fast Lane; 3 November. Wickramasingh, H & Rowley, JA. 2020. How is the Mallampati score used in the evaluation of obstructive sleep apnea (OSA)? Medscape, 15 September.

Crystal Smith is a Senior Education Consultant for Critical Care Education Services (part of the Medcast Group). She has a clinical background in critical care, paediatrics and education.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreFollow James, a 7-year-old boy scheduled for a tonsillectomy and adenoidectomy, as we explore how the 4 P’s of child preparation – Prepare, Play, Parent, Praise – can be used in day surgery to reduce procedural anxiety, support family-centred care, and improve the overall patient experience
Caregiver concern is a powerful predictor of clinical deterioration in children, often surpassing abnormal vital signs. A recent Lancet study confirms its association with ICU admission and ventilation. Integrating caregiver input into assessments, documentation, and escalation protocols can significantly improve early recognition and outcomes in paediatric emergency care.
Sepsis is a time-critical medical emergency. The National Sepsis Program urges GPs and primary care clinicians to enhance early recognition and management of sepsis to save lives. This update outlines key actions and available resources to support timely diagnosis and intervention across primary care settings.
