Clinical Opal #18 - IBS or IBD?
She describes 1-2 loose bowel actions and intermittent crampy abdominal pain most days but denies any blood or mucous in the stool. She says that she feels less hungry and but has not lost any weight. There has been no fever or other constitutional symptoms. She describes a lot of recent stress in her life, both at work and home.
Her past medical history is unremarkable, and she takes no medications. She does not drink alcohol or smoke cigarettes. There is no significant FHx of bowel disease. Her examination is normal.
Two weeks ago Millie had a faecal multiplex PCR test and stool culture, both of which were normal. Baseline blood tests were also normal.
You consider the most likely diagnosis is irritable bowel syndrome (IBS) but are keen to exclude inflammatory bowel disease (IBD). However, you are reluctant to send her off for a colonoscopy as the likelihood of organic disease is low.
Based on Millie’s presentation, what is the role of faecal calprotectin testing?
The symptoms of IBS and IBD overlap significantly and differentiation on clinical grounds can be challenging. As a result, many patients with functional gastrointestinal disease (GID) like IBS are referred for further assessment, including colonoscopy.
Faecal calprotectin (FC) is a neutrophil-derived protein biomarker and is used in clinical practice as a surrogate marker of intestinal inflammation. A recent systematic review and meta-analysis published in the MJA found that FC testing is clinically useful for distinguishing IBD from IBS, with a sensitivity of 88% and specificity of 72%.[i] Assuming a population prevalence of organic GID of 1%, the authors calculated that FC testing has a negative predictive value of 100%.
The Gastroenterological Society of Australia (GESA) clinical guidance on IBD states that FC is ‘highly accurate in distinguishing IBD from IBS’ and states that a negative result (in the absence of alarm features, or abnormal blood or stool tests) effectively precludes the need for further investigations.[ii] See algorithm below.
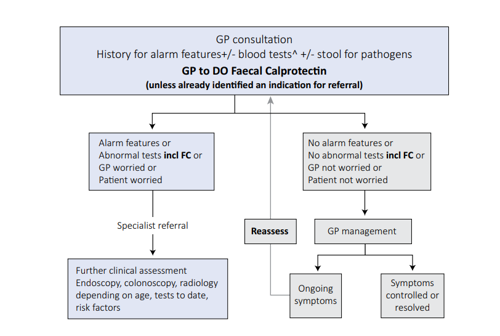
Taken from Gastroenterological Society of Australia Inflammatory Bowel Disease Clinical Update 2018
In older patients (over 40) where the incidence of non-inflammatory organic GID like colorectal cancer starts to increase, a lower threshold for referral of patients with new GI symptoms should always be considered.
References:
[1] An Y-k, et al. Faecal calprotectin testing for identifying patients with organic gastrointestinal disease: systematic review and meta-analysis. MJA 2019. 211;10:461-67.
[2] Gastroenterological Society of Australia Inflammatory Bowel Disease Clinical Update 2018

Simon is a GP based in Newcastle, NSW, and a senior medical educator with Medcast. He also has medical education roles with the RACGP and GPSA.
Over the past three decades, Simon has worked in clinical and educational roles in NSW and the NT, as well as in the Republic of Ireland. He has published over 75 peer reviewed journal articles, and in 2018 received the RACGP Corliss award for his contribution to medical education.
Simon is passionate about high quality education and training. He has particular interests in GP supervisor professional development and the rational use of tests and medicines. He is a proud member of Doctors for the Environment. He spends his spare time drinking craft beer and pretending that he is a musician in the Euthymics, an all-GP band.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreMarjory is a 68 year old in-patient who is 2 days post hip replacement. She is on rivaroxaban (xarelto) for VTE prophylaxis. You find her sitting on the floor of the bathroom, alert but in pain.
We explore the case of Edward, a patient with acute kidney injury (AKI), focusing on renal protection strategies. It explores fluid management, blood pressure control, nephrotoxic drug adjustments, and electrolyte monitoring. Treatment considerations include vasoactive medications, dialysis options like CRRT, and medication dosing to support renal recovery and prevent complications.
James, a university student with a history of seasonal allergic rhinitis, presents with sudden respiratory distress following exposure to grass pollen during a soccer game shortly before a summer thunderstorm. Could this be thunderstorm asthma?
