Tracheostomy Emergencies - Clinical Opal
Sylvia is 62 years old and is self ventilating via her percutaneous tracheostomy which was performed 2 days ago. Sylvia has been in the ICU for 10 days following a MVA where she sustained multiple fractures including bilateral rib fractures. She required prolonged ventilation due to sputum retention. The plan is for her to be discharged to the ward once she is stable.
Sylvia is receiving 2l/min oxygen via her HME (heat moisture exchanger). Her SpO2 has been 95 - 96% all day, with her PaO2 on ABG two hours ago being 90 mmHg. Sylvia has been monitored in SR (Sinus Rhythm) at a rate of 65 - 80 per minute, and her respiratory rate has been 12-16/ min.
What actions should you take?
Firstly it is important to perform an A-E assessment, and escalate as required. As Sylvia has a tracheostomy it is important to assess her airway immediately as it may be blocked. This issue would need to be addressed before continuing the assessment. As you go into the room you notice Sylvia’s secretions are audible, she is tachypnoeic and using accessory muscles of breathing, signs of a partially blocked tracheostomy tube.
You reassure Sylvia that you are going to help her with her breathing. You remove Sylvia’s HME which contains a large amount of slightly blood stained sputum and apply high flow oxygen to Sylvia’s face and tracheostomy. You then remove her inner cannula, which is also partially blocked by sputum. Next you perform tracheal suction which returns a large amount of similar sputum. Once you have ensured Sylvia’s airway is clear, you insert a clean inner cannula and attach a new HME with oxygen as required to keep her SpO2 94-98%.
It is now important to continue the A-E assessment to ensure Sylvia’s airway is now clear, her breathing has improved and that she is cardiovascularly stable.
A tracheostomy tube usually becomes blocked or partially blocked due to inadequate humidification and/or patient hydration leading to thick tenacious sputum, and/or infrequent cleaning of the inner cannula. The use of inner cannulas are recommended as they can be removed to potentially resolve a blockage. Blocked tracheostomy tubes without an inner cannula can only be managed by suctioning or removal of the tracheostomy tube.
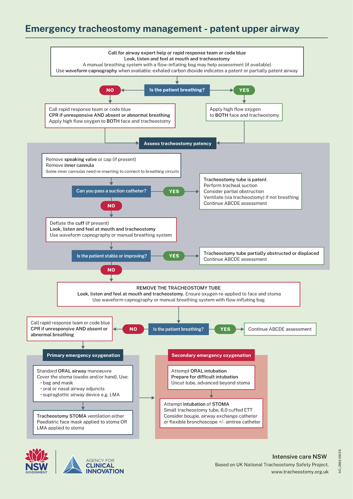
The Agency for Clinical Innovation (2021) highlights that the presence of a tracheal stoma increases the incidence of emergencies and harm to patients. They recommend the use of an emergency algorithm to manage tracheostomy or laryngectomy emergencies. Other causes of tracheostomy emergencies include accidental decannulation, tube displacement, cuff leaks or rupture and airway haemorrhage.
Click to enlarge
Related courses
CCN: Intubation & Tracheostomy Care
Reference
NSW Agency for Clinical Innovation. Care of adult patients in acute care facilities with a tracheostomy: Clinical Practice Guide. Sydney: ACI; 2021

Jenny Browne, RN, Cert IV (TAE), CritCareCert, MN(AdvClinEd), has an extensive background in critical care nursing and education. Jenny has worked across a variety of Australian ICUs, including the John Hunter Hospital (Newcastle), Princess Margaret Hospital (Perth) and the Royal Adelaide Hospital. She has been an ALS and PALS instructor for over 12 years, including with the ACCCN, and is also a sessional academic at the University of Newcastle.
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreCaregiver concern is a powerful predictor of clinical deterioration in children, often surpassing abnormal vital signs. A recent Lancet study confirms its association with ICU admission and ventilation. Integrating caregiver input into assessments, documentation, and escalation protocols can significantly improve early recognition and outcomes in paediatric emergency care.
Sepsis is a time-critical medical emergency. The National Sepsis Program urges GPs and primary care clinicians to enhance early recognition and management of sepsis to save lives. This update outlines key actions and available resources to support timely diagnosis and intervention across primary care settings.
Seeking guidance on which courses to prioritise before the CPD year concludes? You're not alone! Essential CPD for Australian nurses covering skills, patient care & standards.