The Interplay of Long COVID with COPD and Asthma: Implications for Clinical Care
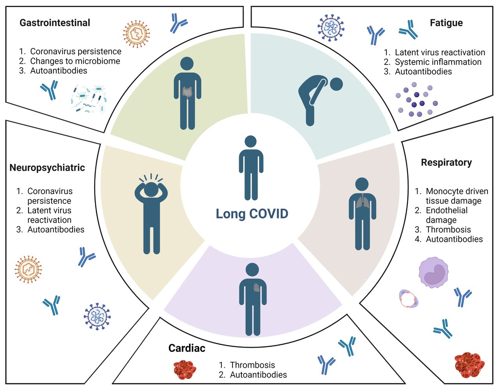
The global emergence of COVID-19, caused by the SARS-CoV-2 virus, has not only presented acute challenges for healthcare professionals worldwide but has also shone a spotlight on its lingering after-effects, colloquially termed "Long COVID". This condition, marked by prolonged symptoms like fatigue, cognitive disturbances, and dyspnea, poses a distinct concern for patients with chronic respiratory conditions like Chronic Obstructive Pulmonary Disease (COPD) and asthma. As our understanding of Long COVID evolves, it is essential to explore its implications for these already vulnerable patient groups.
1. Overlapping Symptoms - Diagnostic Challenges
Dyspnea, or shortness of breath, is a hallmark of both Long COVID and COPD/asthma. For patients with a pre-existing respiratory condition who contract COVID-19, differentiating between an exacerbation of their chronic illness and the continuation of COVID symptoms can be challenging. Healthcare providers must be vigilant in their assessments, perhaps relying more heavily on objective tests such as spirometry or imaging to discern the primary etiological factor.
2. Inflammation and Airway Hyper-responsiveness
Both COVID-19 and asthma are characterised by inflammatory processes, albeit of different origins. There's emerging evidence to suggest that Long COVID might prolong or exacerbate airway inflammation, potentially leading to increased bronchial hyper-responsiveness in asthma patients. For those with COPD, a condition marked by chronic inflammation, the added inflammatory burden of Long COVID may lead to further deterioration of lung function.
3. Treatment Modalities and Therapeutic Implications
The intersection of Long COVID with COPD and asthma may necessitate a reassessment of therapeutic strategies. For instance, a greater emphasis on anti-inflammatory agents or adjusting the dosages of bronchodilators might become necessary. Clinicians may also need to be wary of potential drug interactions if antiviral or other COVID-specific treatments are continued in the long term.
4. Rehabilitation and Pulmonary Function
For those with pre-existing respiratory conditions, pulmonary rehabilitation is a cornerstone of management. With the advent of Long COVID, the demand for specialised rehabilitation programs that cater to both the chronic condition and the lingering effects of the virus is likely to rise. Customising rehabilitation to address the unique challenges posed by the confluence of these conditions will be essential.
5. Mental Health Considerations
The psychological toll of Long COVID is gaining recognition. Given the chronic nature of COPD and asthma and the frequent limitations they impose on quality of life, the added mental health burden of prolonged COVID symptoms can't be ignored. Healthcare providers should be prepared to offer enhanced psychological support or refer patients to mental health specialists as needed.
Conclusion
Long COVID, with its myriad manifestations, is charting new territories in clinical medicine. For patients with COPD and asthma, the journey may be even more intricate. As research on Long COVID continues, it is paramount for healthcare professionals to remain updated, adaptable, and compassionate, ensuring that the best possible care is provided to those navigating these dual challenges.
Related courses
Managing Respiratory Disease in Patients with Long COVID.
References
-
Global Initiative for Chronic Obstructive Lung Disease (GOLD). (2021). Global Strategy for the Diagnosis, Management, and Prevention of COPD.
-
National Heart, Lung, and Blood Institute. (2020). COPD. National Institutes of Health.
-
Australian Government Department of Health. (2020). Chronic Obstructive Pulmonary Disease (COPD). The Australian Lung Foundation.
-
Marshall, M., Howe, A., Howsam, G., Mulholland, M., & Leach, J. (2020). COVID-19: a danger and an opportunity for the future of general practice. The British Journal of General Practice, 70(695), 270-271.
-
Greenhalgh, T., Knight, M., A’Court, C., Buxton, M., & Husain, L. (2020). Management of post-acute COVID-19 in primary care. BMJ, 370.
-
Australian Government Department of Health. (2021). Management and Treatment of Long COVID. Commonwealth of Australia.

Susan is the Head of Nursing Education for the Medcast Group.
DipAppScNsg, BN, CritCareCert, CoronaryCareCert, TraumaNsgCareCert, CertIV(TAE), MN(Ed), and GradCert(Ldrshp & Mgt).
Become a member and get unlimited access to 100s of hours of premium education.
Learn moreGenetic testing in general practice: Dr. Alan Ma explains which tests GPs can order, when to refer, and how the PRECISE portal supports confident testing and referral decisions.
Genomics is now part of everyday general practice. The PRECISE Genomics in Primary Care hub gives Australian GPs fast, practical tools to recognise genetic red flags, guide testing and support timely referrals.
GP Dr Kate Annear and Clinical Psychologist A/Prof Aliza Werner-Seidler discuss practical strategies for engaging young people, conducting psychosocial assessments, and using lifestyle, social, psychological and digital interventions to support mild to moderate depression and anxiety in young people.


